Osteoarthritis
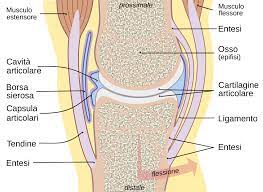
Arthrosis or osteoarthritis (OA) is a chronic joint disease characterized by degenerative and productive lesions of the cartilage of the joints diarthrodial joints. Diarthrosis are joints characterized by a structure aimed at movement. They have cartilage and joint capsule, then membrane and synovial fluid. All these structures, together with the subchondral bone (immediately below the cartilage), may be involved in OA [1].
The prevalence of OA increases with age and the peak frequency appears to be between 75 e i 79 years. In this age group it is mainly found in the cervical spine, in both men and women, of the lumbar spine for men and the interphalangeal joints of the hand for women.
Osteoarthritis of the hand at a radiological level it is highlighted in about 54%-67% in the adult population aged 18 and over 55 years. It is estimated that among people positive to radiographic evidence the 47% will develop osteoarthritis of the distal interphalangeal joints and about the 50% at the level of the proximal interphalangeal joints[2]. That of the hand is the most common type of osteoarthritis and affects 3 times more women than men. In the advanced stages of the pathology they can develop osteophytic formations at the level of the proximal and distal interphalangeal joints giving rise respectively to the characteristics Bouchard and Heberden nodes. Deterioration of joint cartilages by bringing bone ends into direct contact within the joint causes joint pain, swelling and stiffness. In the long run, the pathological process can lead to osteoarticular deformities.

Osteoarthritis can also affect large joints such as the knees (gonartrosi) and the hip (coxartrosi) and in some cases it can lead to the need for arthroplasty surgery.


However, the clinical manifestations of OA are found only in the 30% of OA diagnosed with radiological investigations [3]. The frequency between the two sexes varies according to age (OA in humans is more frequent under i 45 years while in the woman over i 55 years) and topographic distribution, as we have already seen, It is different[4].
OA is considered a disease multifactorial etiopathogenesis, triggered and carried forward by factors that change the state of joint balance. To maintain this balance is necessary, in the first place, the good health of the cartilage, structure necessary to cushion the load on the joints and to protect the bone ends from the friction they would encounter if they worked in direct contact with each other. A fundamental role therefore in the pathological process is played by the load to which the joints are subjected (therefore obesity is also among the risk factors for all the joints that are responsible for supporting the weight of the body against gravity). They also contribute mechanical factors such as joint instability, the traumas, the microtraumas, repeated mechanical stress due to professional activities (lumbarthrosis of drivers…) a sportswoman (coxarthrosis of professional dancers…). In the end, an important role is also played by genetic factors (that involve pathologies that compromise the metabolism or joint function, generating secondary OA: ochronosis, hemochromatosis, familial chondrocalcinosis, dysplasia, the Ehlers-Danlos syndrome, Marfan syndrome, etc.), metabolic disorders (es: diabetes mellitus, hyperuricemia), inflammatory processes, aging[5].






The inflammation seems to play a very important role both in the establishment of the arthritic process and in its progression. Some osteoarthritis is secondary to arthritis, that is, they arise as a consequence of the inflammatory process of inflammation typical of these pathologies. Some inflammatory substances, indeed, are able to influence the metabolism of the cartilage, which can be considered the target tissue of the arthritic process. In the most heavily loaded areas l’osso subcondrale, increases the thickness of the trabeculae as a defense (they are the basic anatomical structure of bone tissue) modifying its density and thus meeting a subchondral bone sclerosis.
They can be formed pseudocyst give geod, probably due to infiltration of synovial fluid, ed osteophytes in the marginal areas of the joint, not subjected to charge.
The joint capsule over time it thickens, reducing the joint's ability to move and hindering venous and lymphatic drainage with damage to metabolic processes. The joint increases in volume, showing a swelling that is usually hard due to the osteophytes. The joint space is reduced due to the gradual thinning of the cartilage (the narrowing of the joint space is noted on the radiographs). In cases of joint effusion the swellings are softer. When moving arthritic joints, their crackling can be heard, due to the irregularity of the articular surfaces, from their contact too close and sometimes from a lack of lubrication. Radiography is the diagnostic imaging par excellence, through which it is possible to highlight the reduction of the joint space, subchondral bone sclerosis, pseudocysts and osteophytes.

The main symptom of osteoarthritis is pain, which is elicited with movement (mechanical pain) and subsides with rest. It is usually absent at night, except in moments in which synovial inflammation is in progress or in the case of concomitant muscle contracture which does not allow a real resting position for the joint. In the morning, or after prolonged inactivity, is present rigidity but its duration, generally of 5-10 minutes, unlike arthritis, does not exceed half an hour.


One of the great problems of OA is given by the fact that the pathology, at the clinical level, manifests itself much later than its onset. Cartilage is devoid of vessels and nerve structures and the absence of the latter deprives the joints of an alarm system, pain, which would allow for timely intervention, especially by changing your lifestyle. It is hypothesized that the irreversibility of the pathology may be due to its late discovery.
There are actually gods supplements that, if caught in time, constantly and for life, they seem to be able to counteract the pathology. Specifically glucosamine, chondroitin and MSM taken concurrently with vitamin C, necessary for their absorption [6] (NOTE: for the use of supplements, contact only your doctor or specialist. What is written in this article is for informational purposes only and for completeness on the subject).


BIBLIOGRAPHY:
[1]German, Silvanus, Pier Franca Gambari, and Leonardo Punzi. Rheumatic diseases. McGraw-Hill, 2007.
[2] Beasley, Jeanine, et al. “Conservative therapeutic interventions for osteoarthritic finger joints: A systematic review.” Journal of Hand Therapy 32.2 (2019): 153-164.
[3]German, Silvanus, Pier Franca Gambari, and Leonardo Punzi. (cit).
[4]German, Silvanus, Pier Franca Gambari, and Leonardo Punzi. (cit).
[5]German, Silvanus, Pier Franca Gambari, and Leonardo Punzi. (cit).
[6] Heather, Olivier, Roy D. Altman, and Jean-Yves Reginster. “Efficacy and safety of glucosamine sulfate in the management of osteoarthritis: evidence from real-life setting trials and surveys.” Seminars in arthritis and rheumatism. Vol. 45. No. 4. WB Saunders, 2016.
Arden, Nigel K., et al. “Non-surgical management of knee osteoarthritis: comparison of ESCEO and OARSI 2019 guidelines.” Nature Reviews Rheumatology 17.1 (2021): 59-66.
Reginster, Jean Yves, and Nicola Veronese. “Highly purified chondroitin sulfate: a literature review on clinical efficacy and pharmacoeconomic aspects in osteoarthritis treatment.” Aging Clinical and Experimental Research 33.1 (2021): 37-47.