Stroke
"Stroke" is a Latin word that literally means "stroke" (in English "stroke") and it underlines the mode of onset of this syndrome that it is, precisely, sudden as a blow.
Among the neurological pathologies, cerebrovascular ones are by far the most frequent. In the population of the most developed countries they are the third leading cause of death (after cardiovascular disease and cancer) and the first cause of disability. Their incidence increases exponentially with age.
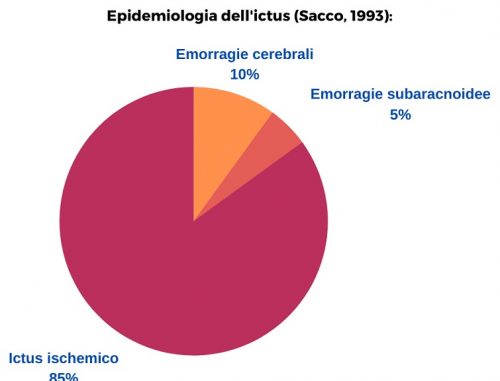
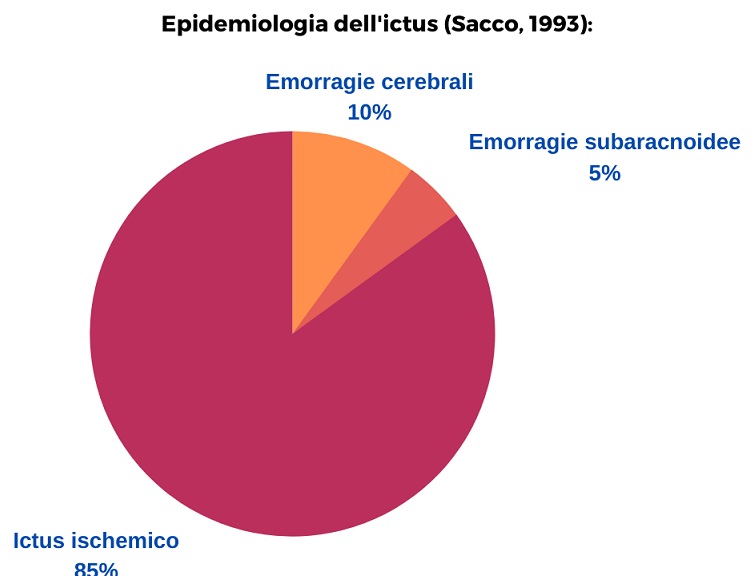
We can distinguish two main types of stroke: ischemic and hemorrhagic. The haemorrhagic stroke then foresee a sub-category which is represented by subarachnoid hemorrhages.
Epidemiology (Sacco 1993):
ISCHEMIC ICTUS
The cause of ischemic stroke is due to an insufficient blood supply in a certain area of the brain (ischemia focale). The lack of blood in this organ leads to different neurological clinical pictures depending on its location. If this lack / absence exceeds a certain time duration, irreversible tissue damage is structured (ischemic stroke or cerebral infarction).
Based on the duration of the symptoms, we can mainly distinguish three types of ischemic vascular events: Transient Ischemic Attack (TIA); Reversible Ischemic Neurological Attack (RIND); Stroke.
If the duration of symptoms is less than 24 hours we talk about Transient Ischemic Attack (TIA: Transient Ischemic Attack). Fazio and Loeb (Fazio-Loeb 2009) they point out that this denomination is highly confusing because it actually looks like 1/3 of patients with TIA actually have signs of brain damage on imaging, despite complete remission of symptoms. Patients who have had a TIA are subject to an increased risk of experiencing an ischemic stroke which, in the first year after the TIA settles around 10% and then go down to 5% annual. The 30% of these patients undergo other TIAs. The percentage of risk is higher in subjects with more than 65 years.
If symptoms last longer than 24 hours but less than three weeks the episode is called RIND (Reversible Ischemic Neurological Attack).
If neurological deficits persist we are talking about stroke. The persistence of neurological deficits is due to the irreversibility of the parenchymal damage caused by prolonged ischemia.
More frequent onset symptoms of cerebral ischemia are:
– Difficulty in speaking (disartria, aphasia)
– Deficit of strength or sensitivity in one side of the body
– Disorder of coordination (ataxia)
– Headache
– Visual disturbances (amaurosi, lateral hemianopia, diplopia)
– Dizziness / skids
Usually the onset takes place during the day, with greater incidence upon awakening or in the early afternoon.
Neurological deficits can have different patterns: they can be complete and stable from the start, manifest in a worsening manner or tend towards improvement. Signs and symptoms that are found on neurological examination allow us to hypothesize the site of the lesion with a good margin of probability, which corresponds to the territory of distribution of the vessel that has undergone occlusion or reduced perfusion. In particular, three syndromes are distinguished: of the anterior or carotid circulation; of the posterior or vertebrobasilar circle; lacunar.
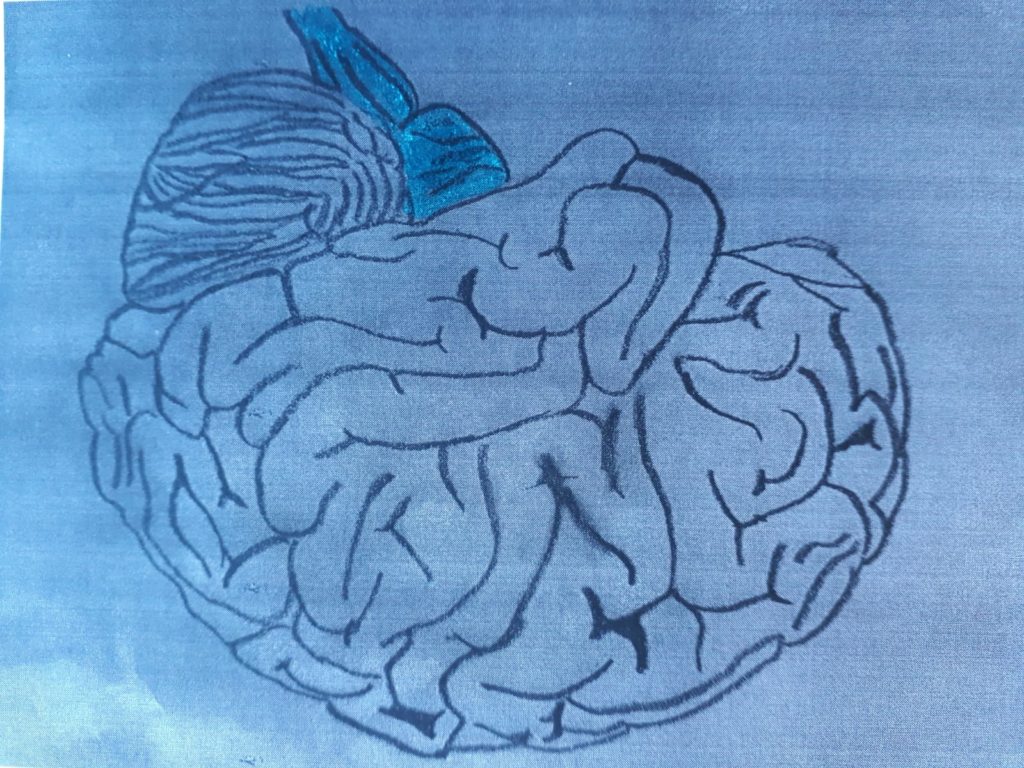
The cerebral circulation is structured in such a way that, in case of obstruction of one of the main arteries (carotids and vertebrals) which lead blood to the brain, its contribution to the entire body is in any case guaranteed: these arteries merge into an arterial ring, the circle or polygon of Willis, from which the blood is distributed to the whole brain.
Anterior circulation or carotid syndrome
Thanks to the circle of Willis, the obstruction of an internal carotid artery can be asymptomatic. In some cases, this precious compensation system can even cushion a bilateral occlusion of both internal carotids. Not always though (for several reasons) this system is able to perform its function. If the circulation of In this case there is an ischemia of the carotid circulation which, depending on its importance, can manifest itself with different clinical pictures that can occur in different combinations:
- hemiparesis / hemiplegia control him (on the opposite side of the body from that of the cerebral insult) which may involve upper limb, lower limb, face;
contralateral homonymous lateral hemianopia;
aphasia for ischemia of the left hemisphere;
forced deviation of the gaze towards the side where the ischemia occurred (it is said that the patient “look at the lesion”);
neglect and other cognitive symptoms (emisomatoagnosia, anosognosia, anosodiaforia) for ischemias affecting the right hemisphere (it should be noted that in a small percentage of the population the hemispheric dominance is reversed between right and left);
disturbances of consciousness
nausea, He retched, hemiataxia, disartria, nystagmus
Posterior circulation or vertebrobasilar syndrome
This syndrome implies that the ischemic insult can involve the occipital lobe, the thalamus, the cerebellum and brain stem.
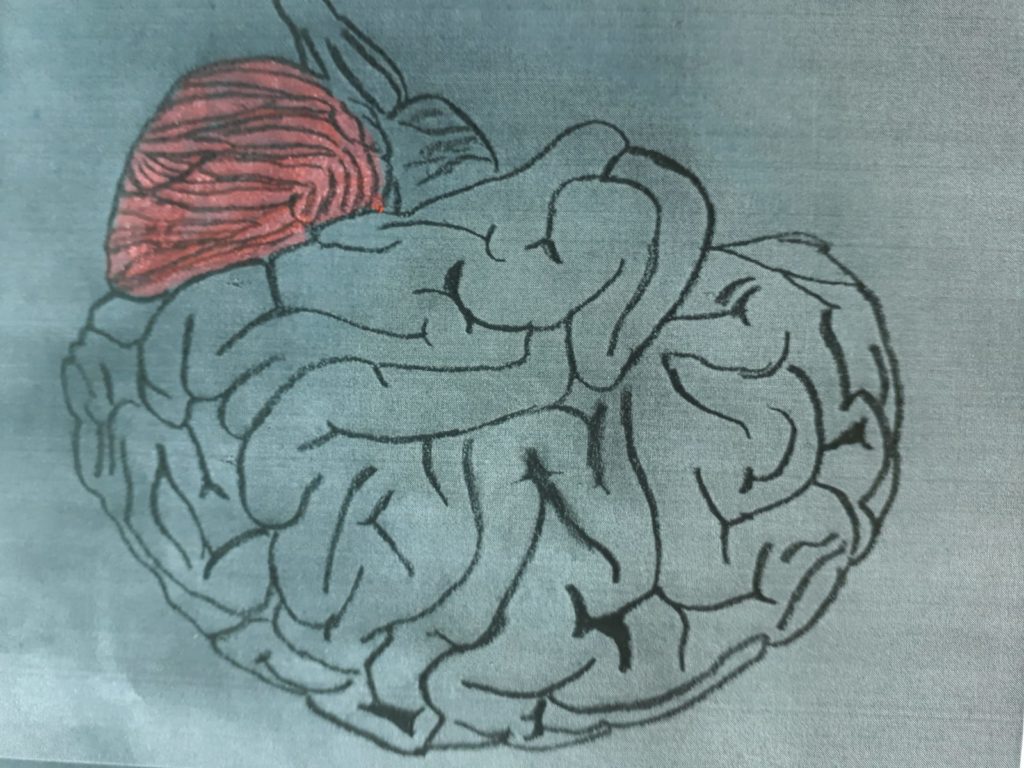
The symptomatology, based on the extent of the lesion, it can involve a variety of symptoms of different types:
visual (occipital lobe)
motors and psychics: contralateral sensory-motor hemisyndrome (lobo occipite).
cognitive visuospatial type (occipital lobe; major thalamic lesions)
bilateral palsy of the III cranial nerve (bilateral ischemia of the thalamus and midbrain)
tetraparesi (bilateral ischemia of the thalamus and midbrain)
aphasia (major thalamic lesions of the left hemisphere)
disturbances of consciousness, visual hallucinations, amnesia (major thalamic lesions)
disartria (cerebellum)
emi-ataxia cerebellar ipsilateral to the lesion (cerebellum)
thermo-pain anesthesia contralateral to the lesion (cerebellum)
dizziness, nystagmus (cerebellum)
peripheral facial paresis (cerebellum)
clinical picture of ischemia of the brainstem, generally not compatible with life.
These are small rounded ischemias (from half a centimeter to one and a half centimeters) which occur in the terminal path of some arteries. They are usually not symptomatic because they occur in areas of the brain that do not produce clinical symptoms in the event of an injury. In some cases though, if they are located in strategic areas of the brain, they can also cause very significant symptoms such as hemiparesis.
RISK FACTORS


The risk factors of ischemic stroke are divided into two main groups. Those "not editable" and "editable". The latter are further divided into two further groups, based on whether the risk attributed to them is certainly documented or not:
Non-modifiable risk factors:
– Age
– Sex
– Familiarity
– Ethnicity
Certainly documented modifiable risk factors:
– Hypertension
– Heart disease
– Cigarette smoke
– Diabetes
– Iperomocisteinemia
– Left ventricular hypoertrophy
– Asymptomatic carotid stenosis
Modifiable risk factors not fully documented:
– Hypercholesterolemia
– Use of oral contraceptives
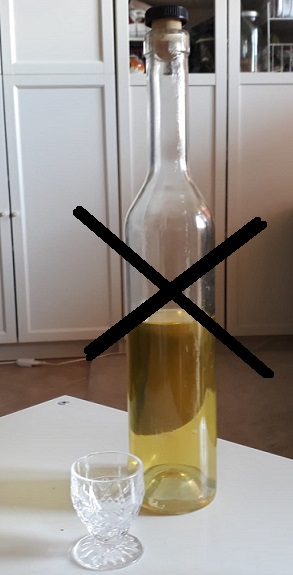
– Alcohol and drug abuse
– Obesity
– Migraine
– Elevated hematocrit
– Medio-intimal thickening of the carotid artery
ETIOLOGY OF ISCHEMIC STROKE:
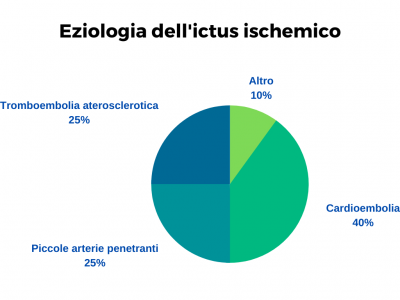
– Atherosclerotic thromboembolism (20-25% of ischemic stroke cases). It occurs due to complications of atherosclerotic lesions of the great epiaortic vessels, of the aortic arch and of the large and medium intracranial arteries: atherosclerotic plaques can give rise to thrombi that limit or occlude the lumen of the vessel, or emboli that detach from the plate and occlude the vessel downstream where its lumen decreasing blocks its passage.
– Cardioembolism (40% of ischemic stroke cases). It can originate from the left atrium of the heart due to the formation of thrombi in this area due to a slowdown in the blood flow inside it (especially in the auricle) which then lead to the detachment of emboli when a greater turbulence of the flow is created (as in the case of intermittent atrial fibrillation); from heart valves when these have undergone pathological processes; from the left ventricle; more rarely from the pulmonary veins, for processes related to oncological pathologies with a pulmonary site.
– Ceric pathologies of the small penetrating arteries of the brain due to hypertension and diabetes. (10-25% of cases of cerebral ischemic episodes). The occlusion of these arteries causes small lacunar infarcts. These are injuries that vary from 2 a 20 millimeters. They are reabsorbed by macrophages (sort of "scavenger cells") and leave small cavities as a result. Lacunar infarcts typically occur deep in the cerebral hemispheres and in the brain stem. They manifest in two main clinical forms. Pure psychic (in lesions involving the thalamus) and pure motor (when the lesions involve the internal capsule or the pyramid of the brain bulb).
PREVENTION
Primary prevention (whose goal is to limit the likelihood that a person who has never had a stroke will be affected) consists ofintervene on modifiable risk factorsi like cigarette smoke, the consumption of alcohol, the decrease in the consumption of salt in the diet, the practice of moderate physical activity, the pharmacological treatment of hypertension and diabetes.




TREATMENT OF ISCHEMIC STROKE
The breakthrough in the treatment of ischemic stroke was determined by the establishment of the Stroke Units and the use of thrombolysis.
It was found that the treatment of the patient with stroke in the Stroke Units significantly reduces both mortality (of about 20%) that disability outcomes in stroke patients (Candelise et al., 2007). The Stroke Units are hospital wards with medical staff, nursing and rehabilitation with specific training for the treatment of stroke patients. Among the reasons for the greater effectiveness of the treatments in the Stroke Units, there is also the fact that these departments are equipped with physiotherapists specialized in neurorehabilitation who ensure early and highly qualified intervention to patients, starting from the positioning that, as we will see later, plays a fundamental role in preventing the establishment of functional limitations but also complications such as the dreaded bedsores.
Regarding the thrombolysis, we can certainly say that it is currently the most popular drug treatment for the hyper-acute phase of stroke. Its use has not only significantly changed the chances of survival of this type of patient but also the degree of residual disability.. However, its effectiveness is linked to compliance with the exclusion criteria that identify the patients for whom it is contraindicated, and the fact that it is administered no later than 4 hours and a half from the stroke. The goal of thrombolysis is the unblocking of the occluded artery with restoration of blood circulation where it was missing. The main risk factor for thrombolysis is the onset of cerebral hemorrhages.
Prognosis
In the former 30 days after stroke, mortality on average is between 10 and the 15%. The 30-40% of surviving patients have disability outcomes.
THE REHABILITATION
Lto rehabilitation of patients with brain damage due to ischemic and hemorrhagic stroke (cerebral haemorrhage and sub-arachnoid haemorrhage), head injuries, provides a first modality of intervention in the acute phase, when the patient is hospitalized in intensive care or in the stroke unit.
After the acute phase then, the neurorehabilitation it may be oriented to the more specific treatment of the different outcomes:
- hemiplegia (including the facial paresis)
- deficit of oculomotor muscles
- speech and language disorders higher cortical functions
- swallowing disorders
HEMORRAGIC STROKE
Epidemiology
Epidemiological hemorrhagic stroke constitutes the 15% of strokes. Mortality, compared to ischemic stroke, it is higher, settling between 35-52% within the first 30 days from the event, half of which within the first two days. Furthermore, only the 20% of the survivors manage to reach a physical and mental condition that allows them an independent life (Steiner et al; 2006; Broderick et al; 2007).
Pathogenesis
Hemorrhagic stroke can be caused by the rupture of a vessel, of a congenital aneurysm, of an Artero-Venous Malformation (MAV)f or a cavernoma.
It occurs most frequently in the deep regions of the brain or cerebellum, in hypertensive subjects. This type of cerebral hemorrhage is referred to as "deep" or "at typical location” (typical stroke). When bleeding occurs in the subcortical white matter, in one of the two lobes of the brain, is called lobar hemorrhage or "at an atypical location” (because it occurs more rarely than the previous one).
Both types usually begin during the day with neurological deficits that worsen within minutes / hours. They often appear disturbances of consciousness and intracranial hypertension symptoms such as headache and vomiting. A fairly clear difference with ischemic stroke and subarachnoid hemorrhage (which we will talk about later), is just the rapid worsening of the clinical picture, modality that in these other typologies is quite rare. However, there are also cases, rare, in which the haemorrhagic stroke evolves asymptomatically.
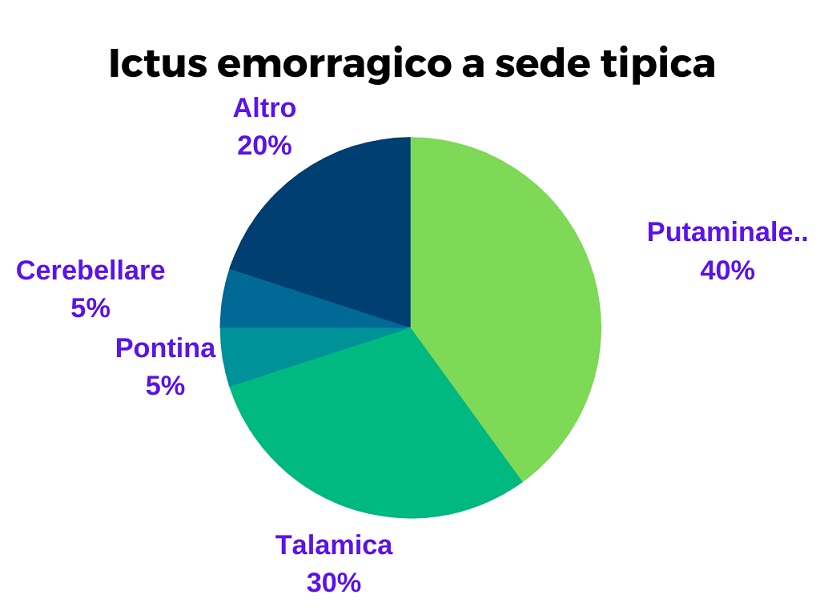
Typical-site stroke (deep or typical bleeding)
Typical hemorrhage is due to rupture of smaller-caliber perforating arterioles that, mechanically stressed by hypertension, they develop fusiform dilations which then go against fissuring. The most affected locations are the nuclei of the base (especially the putamen and the pale) with involvement of the internal capsule, the thalamus, the pons and the cerebellum.
The initial framework of the forms that involve the nuclei of the base and the internal capsule it is mostly characterized by facio-brachio-crural hemiplegia that affects the opposite side to that of the brain injury. In many cases there is a deviation of the gaze and a rotation of the neck towards the side of the brain where the injury occurred. In one third of cases the patient then goes into a coma. When the bleeding is important, it ends up involving the ventricular system. This occurrence leads to symptoms such as headache, vomiting and neck stiffness due to irritation of the meninges and intracranial hypertension that develops due to the involvement of the ventricular system and massive bleeding.
In injuries affecting the nuclei talamici, of small entity, visual disturbances may occur (homonymous lateral hemianopia) neglect (for injuries of the right hemisphere) or speech disorders (fluent aphasia). These deficits in most cases then regress spontaneously. When the damage in this area is greater, there is the possibility that the internal capsule will be compromised and that hemiplegia will consistently occur on the side opposite to the brain injury. The damage can also extend to neighboring structures below the thalamus or to the midbrain resulting in symptoms affecting the intrinsic and extrinsic muscles of the eyes..
If the bleeding occurs at the level of the ponte, in severe cases it can involve quadriplegia and deep coma. In less severe cases, symptoms can vary widely including different types of bilateral motor and sensory deficits or / and cranial nerve impairment., but usually there is no impairment of consciousness.
When the bleeding involves the cerebellum (cerebellar hemorrhage) onset with sudden headache at the nape of the neck, He retched, dizziness and ataxia on the same side of the lesion. A deviation of the gaze to the side opposite the brain injury often appears. In most cases, consciousness is not impaired.
Prognosis
The 30% of patients die within one month of stroke, half of which within the first few days. Impairment of the state of consciousness and the extent of the injury are important predictors.
Thru a seat Infection (lobar or atypical hemorrhage)
It has a better prognosis than the typical seat icuts. It occurs between the cerebral cortex and the white matter in the form of oval-shaped hematomas. The affected brain lobes are, in order of probability, the parietal, the occipital, the frontal and the temporal. The symptomatology, as in all brain damage, depends on the site where the bleeding occurs. The clinical trend in the acute phase shows a succession of worsening in relation to new bleeding events.
SUBARACHNOID HEMORRAGIA (THAT)
It occurs ………………… It is usually due to the rupture of aneurysms or vascular malformations but can also have traumatic causes (head trauma). Sometimes it is the consequence of extensive brain bleeding involving ….
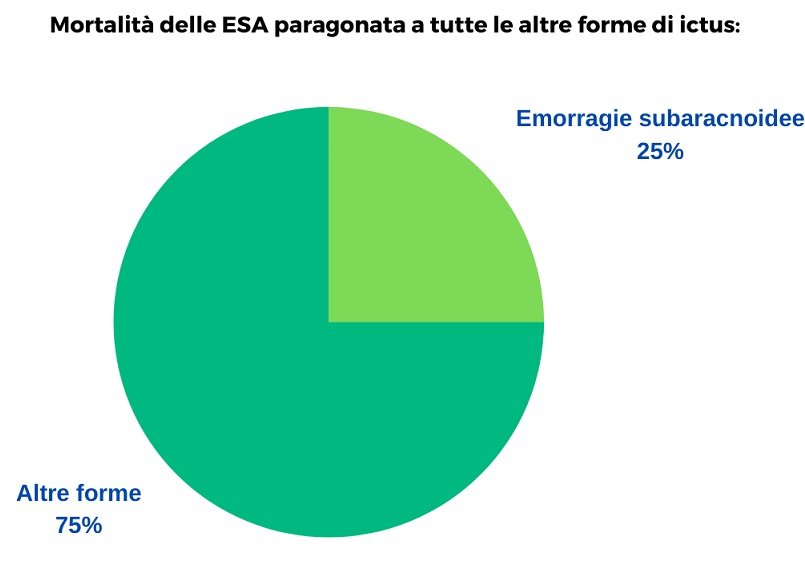
The percentage of sub-arachnoid hemorrhages is very low compared to other forms of stroke but the high mortality that characterizes them makes them responsible for 25% among all stroke deaths, of any type.
Hydrocephalus
Definition of 1978 del WHO (Whorld Health Organization)
Sacco, R.L., 1993, Ischemic stroke is predictable and preventable. New York State,
Fazio-Loeb neurology. Universe Publishing Company. 2009
Candelise et al., 2007; Stroke Unit Trialists’ Collaboration, 2007)