Osteoporosis
Our bones are the result of a continuous process of formation and resorption. When the rate of resorption equals the rate of formation, bone mass remains stable, when, on the other hand, it is greater, the bone mass is reduced. In the second case, when the reduction in bone mineral density or BMD (Bone Mineral Density. E’ a measure of the amount of minerals present in a cubic centimeter of bone) it is milder osteopenia is diagnosed while when a more massive phenomenon occurs we speak of osteoporosis. In osteoporosis, the loss of bone mass leads to a high risk of fractures.
The reduction in BMD may be due to, in women, post-menopause or ovarian failure (type I osteoporosis), in subjects of both sexes it can then be linked to age (type II osteoporosis) or it may result from other etiological factors (secondary osteoporosis)[1]. Secondary osteoporosis may be due to disorders of the endocrine system, ad emopathy, at gastrointestinal diseases, to malnutrition, or the use of certain drugs (corticosteroids, heparin)[2]. There are also forms of juvenile idiopathic osteoporosis.
From the Ministry of Health website we learn that at the epidemiological level:
Science has deepened much knowledge about osteoporosis and is deepening it also through the study of theimpact of space travel on the health of astronauts. During space missions, astronauts find themselves living for a certain period of time outside the influence of the Earth's gravity and, as we'll see, the absence of this stimulus has important physical repercussions on them.

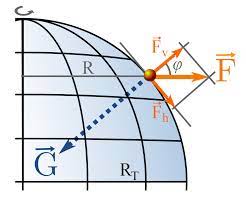
The gravity it is a force which depends on the mass of the bodies, whose intensity is inversely proportional to the distance between the bodies themselves, squared. The earth, by virtue of this force, it pulls us towards the center of its mass. This thing on a proprioceptive level has to do with the sensation we have of the weight of our body, but also of the things we handle or with which we physically relate.

The absence of the force of gravity alters the physiological balance between resorption and production of bone tissue:
si hypothesizes that the absence of the environmental stimulus “severity” behave on the one hand a reduction of osteoblast activity (cells that work on the formation of new bone tissue) and on the other a increased activity of osteoclasts (cells involved in bone resorption) thus determining a negative balance at the level of bone tissue density (osteopenia/osteoporosis). Bones, faced with a reduced workload they reduce their density.
In astronauts, already in the very first weeks of weightlessness there is an increase in calcium levels in the urine (hypercalciuria), a sign that calcium loss from the bones is underway.
At the muscular level, the absence of gravity causes hypotrophy. Muscles too, indeed, having a low workload, reduce their volume.
Lmuscle hypotrophy though, around you, contributes to bone loss, by way of reduced mechanical action of muscles on the skeletal system:
indeed the bones, to maintain the right tissue density, they also need the constant action of adequately strong muscles that subject them to important mechanical stimuli, necessary to solicit the maintenance of an adequately resistant bone structure that can support its intensity.


Our bones therefore need the combined action of gravity and a sufficiently developed muscular system. About the force of gravity, the fundamental thing, however, is that its action is exercised longitudinally on our body, that is, we need to spend a certain number of hours carrying out activities standing upright. Among the problems that occur in the event of long periods of lodging [3] indeed, the strong loss of bone mass is found.


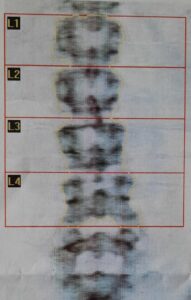
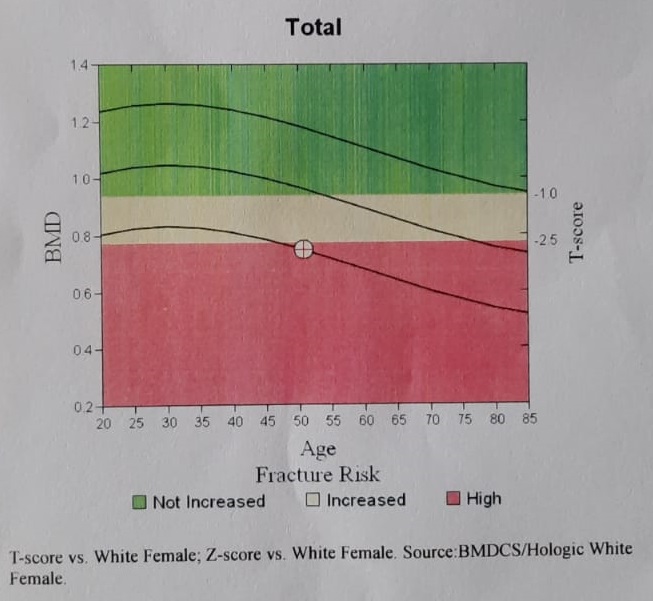
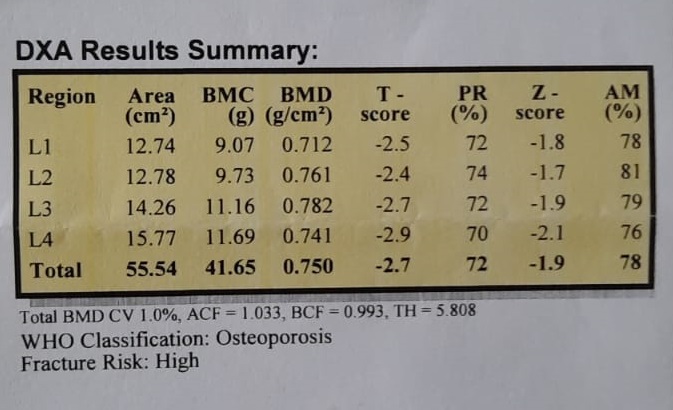
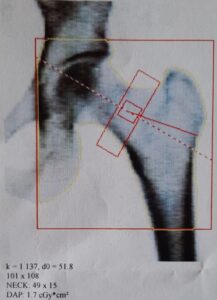
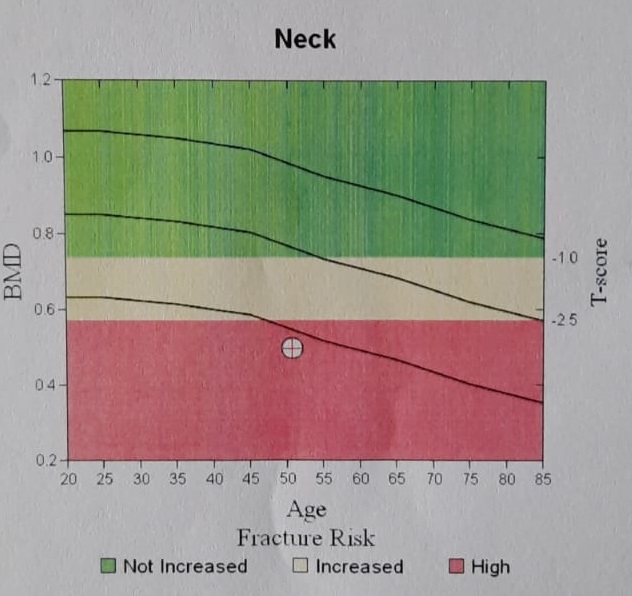
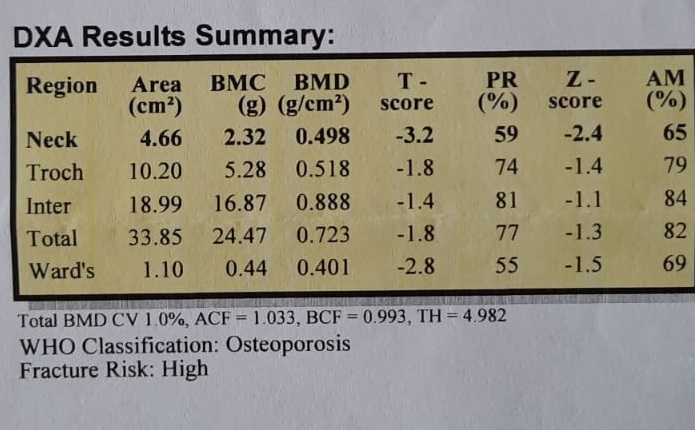
The diagnosis of osteoporosis is done by MOC (Computerized bone mineralometry), a diagnostic imaging method that allows you to appreciate even slight bone loss. The relief is carried out at the level of the femur and lumbar spine.
PHYSIOTHERAPY
As we have seen previously, so that our bones can maintain an adequate state of health, it is necessary that they are regularly subjected to specific mechanical stresses[4], the intensity of which must obviously be calibrated in relation to the bone biomechanical possibilities of each one. Numerous clinical studies have extensively demonstrated that muscle-strengthening exercises can lead to an increase in the mineral density of the bones to which the trained muscles are connected[5] is that, Consequently, pProperly designed exercise programs can counteract the reduction in BMD [6], improve the quality of life of patients and reduce their risk of fractures [7].
L”Physical exercise is now an integral part of the treatment of patients with osteoporosis. In general, an exercise program should include improving general flexibility as one of its goals, of balance, of muscle strength, of trunk stability, gait stability and cardiovascular fitness[8].
[1] Cinnabar, Mehrsheed. “Exercise and osteoporosis.” Archives of physical medicine and rehabilitation 70.3 (1989): 220-229.
[2] German, Silvanus, Pier Franca Gambari, and Leonardo Punzi. Rheumatic diseases. McGraw-Hill, 2007.
[3] Takata, Shinjiro, and Natsuo Yasui. “Disuse osteoporosis.” Journal of Medical Investigation 48.3/4 (2001): 147-156.
[4] Cinnabar, Mehrsheed, et al. “The role of exercise in the treatment of osteoporosis.” Current osteoporosis reports 8.3 (2010): 138-144.
[5] Cinnabar, Mehrsheed. “Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention.” PM&R 4.11 (2012): 882-888.
[6] Cinnabar, Mehrsheed, et al. (Cit. 2)
[7] Cinnabar, Mehrsheed. (Cit. 3)
[8] Cinnabar, Mehrsheed. (Cit. 3)
SINAKI, MEHRSHEED, et al. “Efficacy of nonloading exercises in prevention of vertebral bone loss in postmenopausal women: a controlled trial.” Mayo Clinic Proceedings. Vol. 64. No. 7. Elsevier, 1989.
Cinnabar, Mehrsheed, et al. “Can strong back extensors prevent vertebral fractures in women with osteoporosis?.” Mayo Clinic Proceedings. Vol. 71. No. 10. Elsevier, 1996.
Kai, Ming Chan, Mary Anderson, and Edith MC Lau. “Exercise interventions: defusing the world’s osteoporosis time bomb.” Bulletin of the World Health Organization 81.11 (2003): 827-830.
Cinnabar, Mehrsheed. “Musculoskeletal Challenges of Osteoporosis: Therapeutic Exercise/Strength Training A Review.” From the World of Osteoporosis/Turkiye Osteoporoz Dunyasindan 15.2 (2009)
Improving musculoskeletal health in patients with osteoporosis (https://www.mayoclinic.org/medical-professionals/physical-medicine-rehabilitation/news/improving-musculoskeletal-health-in-patients-with-osteoporosis/mac-20430142)