Multiple sclerosis
It is a pathology that affects the central nervous system that has a dual component: autoimmune-inflammatory and neurodegenerative type. MS is a chronic demyelinating disease that mainly affects the white matter of the CNS with an inflammatory process that determines the formation of sclerotic plaques. White matter plaques can occur anywhere on the CNS (brain and medulla). The most frequently affected areas are the periventricular regions, the corpus callosum, the brain stem, the cerebellum and the posterior or anterolateral cords of the spinal cord (Calabrese et al, 2010). The neurodegenerative component is secondary to the demyelinating effect of the autoimmune-inflammatory attack and involves impairments of the neuronal bodies and therefore, in this case, borne by the gray matter.
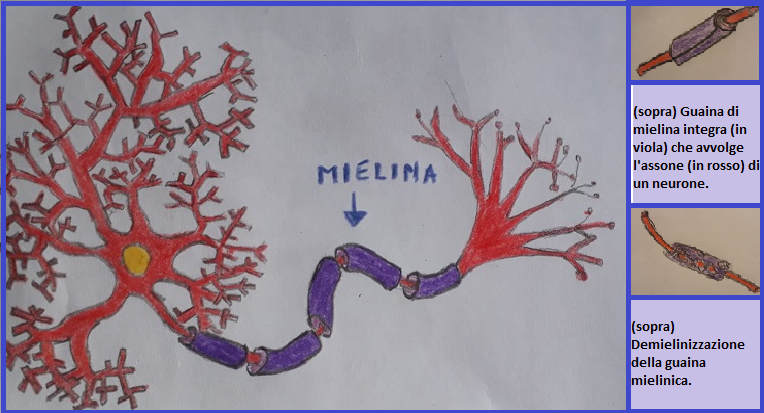
The pathophysiology of MS it is linked to the role myelin plays in the CNS. Myelin is a protective sheath formed by the cytoplasmic membranes of specialized cells (oligodendrocytes) which envelop the axons of neurons. This coating serves to isolate the axons from the surrounding environment to avoid interference in the conduction of the nerve impulse, which is an electrical type signal. Thanks to this coating, the nerve impulse travels very quickly. The demyelination of the axons gives rise to a dispersion of the electrical signal which is slowed down to 20 times compared to the norm up to a total block of the conduction. It has been hypothesized that this slowdown may be the cause of one of the most recurrent symptoms of this disease, namely the "fatigue” (Kos et al, 2008).
The sclerotic plaques that form as a result of the inflammatory process of the white matter, they may vary in size and shape. The more recent ones have more blurred outlines and are edematous and inflamed (ACTIVE ACUTE PLATES). Over time they evolve into a chronic form (ACTIVE CHRONIC PLATE) in which we observe that the destruction of myelin has occurred. The process ends with a reparative cellular reaction (gliosi astrocitaria) which forms a scar area in an attempt to repair tissue damage. In this last stage we speak of CHRONIC SILENT PLAQUE, harder consistency, compared to active plaques, and well-defined outlines.
The etiopathogenesis it is currently still under study. At the moment, research suggests the existence of a multifactorial etiology (a genetic susceptibility and environmental factors). One of the most accredited hypotheses is that of molecular mimicry: a structural affinity between some antigens present in myelin and antigens of external agents such as viruses and bacteria. Immunoglobulin (Ig) produced by the immune system for defense against some external agents would thus also affect the myelin of the central nervous system.
In this interpretation, the pathogenesis would therefore be of the autoimmune type. When Ig bind myelin antigens, they also activate T lymphocytes and macrophages that destroy myelin. This process is then self-fueled by the production of proinflammatory cytokines (TNF, THE 1, ..) which increase local inflammation by recalling other inflammatory cells.
In the initial phase of this pathology the patient experiences a loss of function (the type depends on which area of the CNS is affected) caused by edema and the inflammatory process. With the regression of edema and inflammation we enter the phase of remission of the disease.
Even in the most advanced stages (chronic-progressive phase) there is usually a remission of the acute inflammatory process, but a chronic tissue lesion remains due to reactive gliosis with the formation of scarring areas with real irreversible axonal damage. In this phase, the neuromotor deficit stabilizes and there is no more regression of symptoms.
The progress of MS is defined as "a poussés" with periods of recovery and remyelination AND IT IS RIGHT IN THESE MOMENTS THAT IT IS FUNDAMENTAL TO PERFORM NEURORIABILITATION.
CLINICAL FORMS:
- MONOSINTOMATICA (clinical isolate sindrom, CIS): is characterized by a symptomatic episode lasting at least 24 hours linked to a CNS demyelination. The incidence of this form is approximately 20%.
- RECEIVER-SENDER (Relapsing-remitting). Characterized by the alternation of acute phases and phases of total or partial remission of symptoms in which the disease does not progress at all. The duration of the phases of remission is variable. In 80% of cases during the acute phase there is the appearance of a symptom that reaches its peak after about two weeks and then regresses within two months. In 50% of cases this form evolves towards the secondary progressive form (secondary progressive) after an average of ten years from the onset of the disease. The incidence is of 5%.
- SECONDLY PROGRESSIVE (secondary progressive). It is characterized by a progressive worsening of symptoms and therefore disability without remission. It is an evolution of the exacerbating-remitting form that occurs after an average of ten years from the onset of the disease.
- PROGRESSIVE PRIMARY (primary progressive). The progression of symptoms is slow but is established from the onset of the disease in a gradual manner without pauses. In this form we cannot speak of neuromotor recovery but of slowing down the deficits. This form tends to have a later onset, same frequency in men and women. The incidence of is of 15% circa.
- RADIOLOGICALLY ISOLATED SYNDROME (Radiologically Isolated Syndrome, RIS). These are cases in which they are found, at the level of the CNS, typical MS lesions in the absence of symptoms.
SYMPTOMS - PRIMARY DISORDERS
- Ipostenia. It is due to the impairment of the central motor pathways. Distribution depends on the location of the plaques, which often involves multifocal clinical pictures. The symptom manifested by the patient is usually a feeling of fatigue, even at rest. Fortunately, rehabilitation strongly affects this symptomatology by reducing its severity.
- Ipertonia. It consists in increasing the basic muscle tone (that is, when the muscle is at rest) and involves greater resistance to passive mobilization due to an accentuation of bone reflexes- tendon (or stretch reflexes) which are activated in response to muscle strain. It can also involve the presence of spasms and clones and cause contractures. Hypertonia reduces mobility, negatively affects walking (when the lower limbs are affected) and on the quality of the movement as a whole, resulting in a decrease in dexterity.
- Disturbances in walking. They can result from alterations in muscle tone due to lesions of the pyramidal or extrapyramidal system, but also from an alteration of proprioception or from lesions of the cerebellum. In the latter two cases, balance problems arise that involve widening the support base and postural instability. The main gaits found in MS patients are the scythe and spastic ataxis and derive from the different combination of lesions.
- Fatigue.
SECONDARY DISORDERS
- Contractures.
- Lower back pain. The 20% it is of the primary type for neuritis due to a plaque at the root level or in the meninges of the spinal cord while 80% is secondary to hernias or disc protrusions caused by an alteration in the patient's posture.
- Disorders of urination. The bladder is a sac with muscular walls (detrusor muscle) which are subjected to an extremely refined and very complex control by the central nervous system because it is divided into several levels. A lesion at any point of this system can alter bladder control leading to different symptoms that can range from incontinence to bladder stagnation with the risk of urogenital infections.
- Disorders of swallowing.
- Restrictive respiratory syndrome. It occurs when the altered tone and weakness affect the respiratory muscles.
- Speech disorders. The type of these disorders depends on the location of the lesion.
- Cognitive impairment. This term refers to those deficits affecting the higher cortical functions (attention, memory, language, planning skills, problem solving, visual-spatial functions ...)
Calabrese M et al. Imagine distribution and frequency of cortical lesions in patients with multiple sclerosis. Neurology 2010
Kos, D., Kerckhofs, E., Nails, G., D’hooghe, M.B., & Ilsbroukx, S. (2008). Origin of fatigue in multiple sclerosis: review of the literature. Neurorehabilitation and neural repair, 22(1), 91-100.